[lwptoc]
1. Introduction
Bed sores, also known as pressure ulcers, pose a significant challenge in caregiving, especially for those providing round-the-clock care to individuals who are bedridden or have limited mobility.
These painful skin and tissue injuries are not only discomforting for the patient. They can also lead to severe complications if not addressed promptly and effectively.
Bed sores arise from prolonged pressure exerted on specific body parts, disrupting the normal blood flow to the skin. Most common in bony areas, these sores can significantly reduce a patient’s quality of life, making every move a painful ordeal.
However, with the proper knowledge, consistency, and patience, caregivers can help prevent these troublesome sores from developing and ensure their loved ones are comfortable and pain-free.
This guide will dive deep into understanding the causes and signs of bed sores and how to prevent them effectively.
We will also explore some treatment strategies and the crucial role of professional care in managing these sores.
Filled with practical tips and real-life examples, this guide aims to equip caregivers with the knowledge they need to care for their loved ones.
So, let’s tackle this challenging caregiving hurdle head-on!

Image by Nattanan Kanchanaprat from Pixabay
2. The Underlying Causes of Bed Sores
Understanding the causes of bed sores is the first step toward effective prevention and treatment.
Bed sores, or pressure ulcers, develop due to prolonged pressure or friction on the skin, usually in areas overlying bony prominences such as the elbows, heels, hips, and tailbone.
The main culprit is sustained pressure, which can arise from long periods of immobility or inactivity.
When an individual stays in one position for extended periods, the pressure exerted on the skin by their body weight limits blood circulation to the skin and underlying tissues.
This restricted blood flow deprives the skin cells of necessary oxygen and nutrients, leading to cell death and the formation of sores.
Aside from constant pressure, other factors also contribute to bed sore development.
Shear is one such factor when two surfaces slide in opposite directions. For instance, when a bedridden individual slides down a bed, the skin over a bony area may stay in place.
At the same time, the deep tissue moves downwards with the skeleton. This motion can stretch and tear blood vessels, aggravating skin vulnerability and promoting bed sores.
Friction is another element that can cause or exacerbate bed sores. This occurs when the skin rubs against clothing or bedding, leading to skin weakening and irritation, especially in moist conditions.
People with fragile or damp skin are particularly susceptible to damage from friction.
Moreover, underlying health conditions can increase the risk of bed sores. Poor nutrition and dehydration can affect skin health and resilience, making the skin more susceptible to damage.
Similarly, conditions that limit mobility or sensation, such as spinal cord injuries, can heighten bed sore risk because individuals may not feel discomfort or pain that would otherwise prompt them to move.
By understanding these root causes, caregivers can be more proactive in spotting potential risks and taking preventative measures to ensure their loved one’s comfort and well-being.
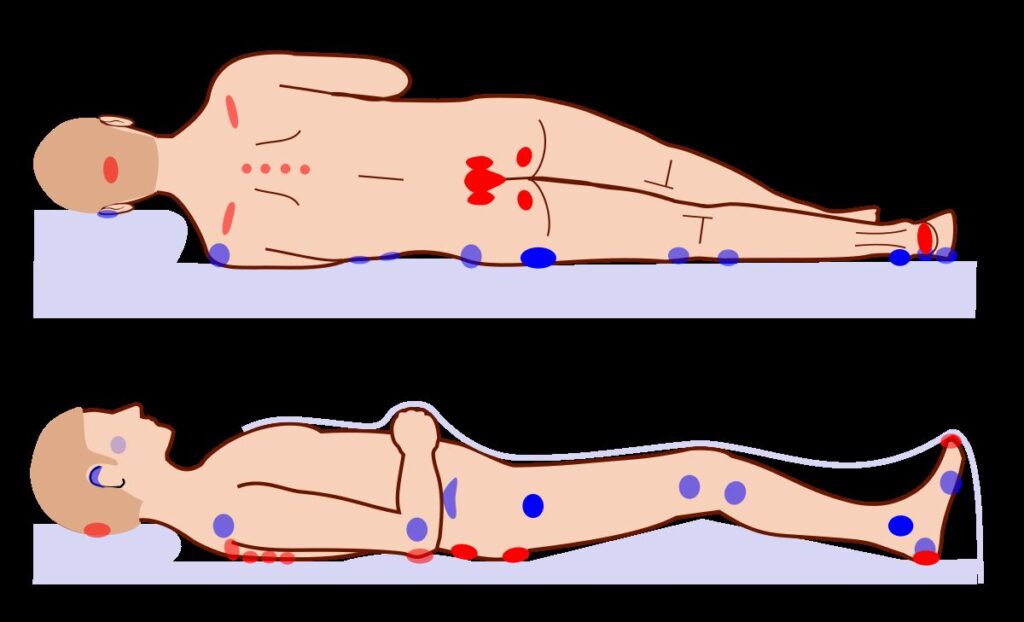
File:Pressure ulcer points.svg. In Wikipedia.
3. Bed Sores: The Warning Signs
Recognizing the early warning signs of bed sores is critical to prevent their progression. Bed sores typically develop in four stages, each with distinct symptoms.
Stage one is the mildest form, where the skin is still intact but may appear red or discolored, especially in people with lighter skin tones.
For individuals with darker skin, the skin may not look red. Still, it could be a different color than the surrounding skin, feel warmer or cooler to the touch, or have an unusual texture. The area might also feel either firmer or softer than the surrounding skin.
By stage two, the skin might be damaged or lost, exposing a layer of the skin underneath. The sore may look like a scrape, blister, or shallow crater in the skin. The area around it might feel warm, swollen, or painful.
In the later stages (three and four), the damage extends deeper into the tissue, potentially exposing muscle, bone, or tendons. The sore could look like a deep wound or crater, and there might be signs of infection like pus, odor, heat, or red edges.
Early detection is vital in bed sore management. Awareness of these signs enables caregivers to initiate immediate action and medical intervention to mitigate further complications.
Stages of pressure ulcer. Source: New Zealand Wound Care Society.
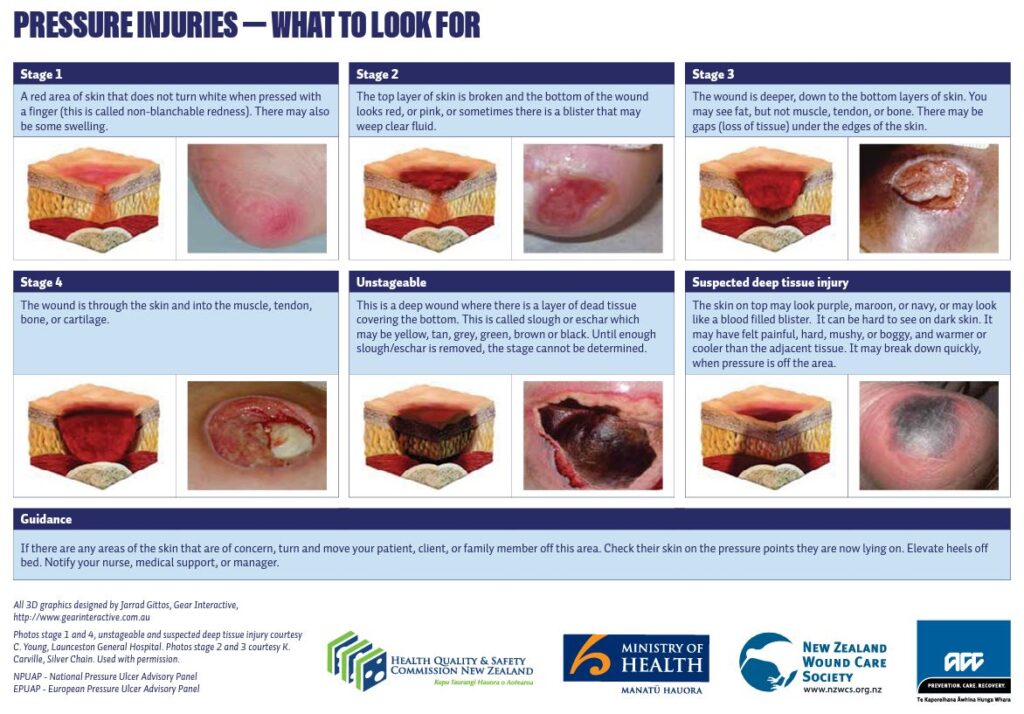
Stages of pressure ulcer. Courtesy of New Zealand Wound Care Society.
4. Tip #1: Regular Repositioning
Regular repositioning is one of the most effective ways to prevent bed sores. When an individual spends extended periods sitting or lying down, pressure builds up on specific body areas, such as the hips, lower back, heels, and tailbone.
Regularly shifting their position can help alleviate this pressure, promoting better blood circulation and, thus, reducing the risk of bed sores.
For individuals confined to a bed, repositioning should occur approximately every two hours.
Caregivers can alternate the person’s position between lying on their back, left, and right sides, using pillows to support and protect bony areas.
Consider investing in specialized mattresses or overlays designed to redistribute pressure more evenly.
Below is a video on bed repositioning.
For those who use a wheelchair, aim to shift the person’s weight approximately every 15 minutes.
Assist them in leaning forward, sideways, or performing small lifts from the seat if possible. Encourage them to stretch regularly and exercise exercises that promote circulation.
Importantly, repositioning should be done gently to avoid causing friction or shear, as these can also contribute to bed sore development.
Seeking advice from healthcare professionals on correct repositioning techniques can ensure safety and effectiveness in this preventative strategy.
5. Tip #2: Proper Hygiene and Skin Care
Keeping the skin clean and dry is pivotal in preventing bed sores. Moisture from sweat, urine, or feces can break down the skin and increase the susceptibility to pressure sores.
Regular bathing, preferably with warm water and mild soap, can help keep the skin clean. However, over-bathing can lead to dryness, which may also increase the risk of skin breakdown.
Striking a balance is essential – aim for a routine that maintains cleanliness without compromising the skin’s natural moisture.
After bathing, gently pat the skin dry, taking extra care not to rub or create friction.
Daily inspections of the skin should also be part of this routine. Look for changes in color, temperature, or swelling, as these could be early indicators of a pressure sore.
Proper nutrition and hydration also contribute significantly to skin health. Ensure the person drinks ample water and consumes a balanced diet enriched with proteins, vitamins, and minerals.
Finally, moisture-barrier creams can be considered, particularly in areas prone to excessive moisture (from urine or feces). These creams provide a protective layer that can help prevent skin irritation and breakdown.
Always consult with healthcare professionals for appropriate products tailored to individual needs.
6. Tip #3: Quality Nutrition and Hydration
Maintaining proper nutrition and hydration is fundamental to bed sore prevention. A well-balanced diet can enhance overall health, boost the immune system, and improve skin resilience, reducing susceptibility to pressure sores.
The significance of protein in the diet cannot be overstated regarding wound healing and skin health. The diet includes excellent lean protein sources, such as chicken, fish, eggs, and legumes.
Vitamins and minerals play crucial roles too. Vitamin C and zinc, particularly, facilitate skin regeneration and wound healing.
Citrus fruits, strawberries, and bell peppers are good sources of Vitamin C, while zinc can be found in foods like seafood, meats, seeds, and nuts.
Hydration is another critical aspect. Drinking sufficient water keeps the skin supple and resilient, reducing skin breakdown risk.
But remember, it’s not just about water. Fluids can also come from other sources, such as fruits, soups, and teas.
However, nutritional needs can vary from person to person, and it’s recommended to work with a registered dietitian or a healthcare provider who can provide personalized advice considering existing health conditions and dietary preferences.
Nutrition isn’t a one-size-fits-all scenario, and personalization is critical for effectiveness.

Image by Gábor Adonyi from Pixabay
7. Tip #4: Pressure-Relieving Devices
Regarding preventing bed sores, the adage ‘prevention is better than cure’ fits perfectly. An essential part of this prevention strategy is the use of pressure-relieving devices.
These devices, often used with regular repositioning, can significantly reduce the risk of bed sore development in those with limited mobility.
Pressure-relieving devices are specially designed to distribute body weight and reduce pressure on vulnerable areas evenly. Many of these devices are available today, each with its own merits and suited to different needs.
Pressure-relieving mattresses, also known as pressure redistribution mattresses, are one such device.
These mattresses are made from high-density foam, air, or gel, providing a cushioning effect that helps redistribute pressure.
For instance, an air-filled alternating-pressure mattress continuously inflates and deflates air cells to shift pressure regularly, preventing sustained pressure on any area.
Cushions are another helpful device. Whether they’re made of foam, gel, or air, these cushions can be used on regular chairs, wheelchairs, or even car seats, offering protection in bed and during daytime activities.
Then there are pressure-relieving overlays, which can be placed atop a standard mattress. Overlays are an economical option for those unable to invest in a special mattress. They can offer a similar degree of protection.
Inflatable limb protectors can help reduce pressure on specific body parts like heels or elbows, which are highly susceptible to bed sores due to their bony prominence.
Remember, not all devices are created equal, and what works best depends on individual needs, immobility, and other health conditions.
It’s always best to consult with a healthcare professional or an occupational therapist who can provide advice tailored to the individual’s circumstances.
The appropriate pressure-relieving device can make a significant difference in the battle against bed sores.

Image by congerdesign from Pixabay
8. Treatment Strategies for Bed Sores
When dealing with bed sores, various treatment strategies come into play.
However, the focus here will be narrowed down to three specific areas: wound dressings, infection management, and, when necessary, surgical interventions.
Wound dressings, the first line of defense against severe bed sores, provide a moist healing environment that accelerates recovery. A myriad of dressing options is available, with the choice greatly dependent on the stage and condition of the bed sore.
Hydrocolloid and foam dressings are commonly used for early-stage sores, while alginate dressings, loaded with seaweed derivatives, can absorb exudate from more advanced wounds.
Other cutting-edge dressings, like those containing silver or honey, have antimicrobial properties which help stave off infections.
Speaking of infections, they pose one of the most substantial risks in bed sore management.
If a bed sore becomes infected, it can lead to complications such as cellulitis or sepsis, potentially life-threatening conditions.
To combat this, doctors may prescribe topical or oral antibiotics. If the infection is deep or severe, intravenous antibiotics may be required. Routine wound cleaning with a saline solution can also help prevent infections from setting in.
Surgical intervention might be considered in extreme cases where the bed sores have progressed extensively.
One surgical option is debridement, where dead tissue is surgically removed to allow healthy tissue to heal.
Flap reconstruction is another method for moving healthy skin to cover the area where the bed sore was removed.
In dire cases where the infection has reached the bone in the extremities and is life-threatening, amputation might be a necessary recourse.
These focused treatment methods underline the gravity of bed sores and the extensive medical interventions they may necessitate. This highlights the need for early detection, proactive care, and timely treatment to manage this significant health concern.

Image by Mar Dais from Pixabay
9. The Crucial Part Professional Care Plays in Managing Bed Sores
Professional care in managing bed sores cannot be overstated, with experts bringing an array of critical skills and experience to bear in detecting, preventing, and treating these painful wounds.
Firstly, healthcare professionals, such as nurses and doctors, can identify the early signs of bed sores.
Regular skin assessments by these experts are fundamental to early detection and prevention, averting the painful and potentially life-threatening complications that can ensue from advanced bed sores.
Moreover, professionals play an essential role in developing a personalized care plan.
With a comprehensive understanding of an individual’s health status, activity level, and nutrition needs, they tailor preventive measures to suit the person’s unique circumstances.
These plans often encompass repositioning schedules, dietary recommendations, and skincare routines, all aimed at preventing the onset of bed sores.
In cases where bed sores have developed, healthcare professionals are skilled in administering proper wound care and treatment methods.
Their expertise is indispensable, from determining the appropriate wound dressings to managing infections and prescribing necessary medications. In severe cases, they collaborate with surgeons to facilitate essential surgical interventions.
Professional care forms the backbone of practical bed sore management, underscoring the significance of professional input at each stage: prevention, detection, and treatment.
10. Real-life Case Study: Mary’s Challenge and Triumph Over Bed Sores
Let’s delve into a real-life story that illustrates the struggle and ultimate success in managing bed sores.
Meet Mary, a dedicated caregiver for her 80-year-old mother, Lillian, who has been bedridden due to severe arthritis.
Initially, Mary was unaware of the risk of bed sores until she noticed a red, irritated area on her mother’s lower back. After consulting a healthcare professional, they confirmed it as a stage one pressure ulcer, commonly known as a bed sore.
Mary was distressed, but she decided to take proactive steps.
She invested in pressure-relieving devices, including a high-quality pressure mattress and cushions. She also strictly repositioned her mother every two hours, monitored hydration and nutritional needs, and maintained diligent skin care.
When Lillian’s bed sore showed signs of infection, Mary promptly sought medical treatment. The healthcare provider prescribed topical and oral antibiotics to combat the infection and recommended specialized dressings for wound healing.
With patience, commitment, and perseverance, Mary managed to not only treat the existing bed sore but also prevent any new ones from forming.
Lillian’s quality of life improved noticeably, a testament to the impact well-informed and dedicated caregiving can have on bed sore management.

Image by Manuel Alvarez from Pixabay
11. Conclusion: Be Vigilant, Stay Proactive
In closing, understanding, preventing, and treating bed sores isn’t solely a medical pursuit but a collective responsibility shared by caregivers, family members, and health professionals.
These sores, while common among immobile individuals, aren’t inevitable.
We can significantly reduce the likelihood of their occurrence by remaining vigilant for early warning signs and adopting proactive, practical strategies such as regular repositioning, meticulous hygiene, and proper nutrition.
Even when bed sores do develop, we are not without recourse. A host of effective treatment strategies, from specialized wound dressings to advanced surgical interventions, are available.
However, prevention remains the best cure, necessitating continued dedication to high-quality care for those at risk.
Remember that caring for someone prone to bed sores can be challenging, but you are not alone. Professional care is always available to lend their expertise, support, and encouragement in this fight against bed sores.
After all, every step toward better understanding and managing bed sores is toward improved quality of life for our loved ones.




